By Barry Keate
Barry Keate, has lived with tinnitus over 40 years and has published 150+ research articles on numerous aspects of tinnitus. He is an expert on the condition and a well-known advocate for those with tinnitus.
For decades scientists have attempted to understand the complexities of tinnitus. One of the primary tools for basic research has been the use of brain scans in an attempt to locate the exact part of the brain that causes tinnitus. Meetings of the International Tinnitus Forum are replete with thousands of brain scans showing highlighted areas of the brain thought to be responsible for the phantom sound.
Until recently, brain scan imaging has not shown a high degree of accuracy. Entire hemispheres of the auditory cortex show increased neural activity. This is not helpful for pinpointing exact areas to target for interventional therapy. Potential therapies include electrical, chemical, pharmaceutical and nutraceutical interventions. A much more precise method is required in order to facilitate understanding and aid in targeting tinnitus therapy.
Now, a relatively new imaging technique, Magnetoencephalography (MEG) has emerged as a procedure that brings tinnitus imaging into much sharper focus.
MEG measures the minute magnetic fields that are generated by electrical activity in the brain. It is completely non-invasive and does not require the use of ionizing radiation or injected radioactive dyes used in other imaging technologies. It is also quiet, as opposed to MRI, which requires earplugs. And, best of all, it is able to pinpoint areas of excess neural activity as small as 2 mm (less than 1/10 inch) in diameter.
A brief review of other brain imaging techniques reveals two basic forms of brain scans; structural and functional. Structural imaging looks for structures and shapes in the brain such as inflammation, tumors or blood clots leading to stroke. Functional imaging looks to determine what areas of the brain are most active during a particular stimulus. The active brain areas become brighter on the scan and are referred to as “lighting up.”
Structural Imaging
Computed Tomography (CT or CAT) scans use a series of x-rays of the head. These scans are used primarily to evaluate the degree of swelling from tissue damage.
Magnetic Resonance Imaging (MRI) scans use magnetic fields and radio waves to produce high quality images of brain structures without the ionizing radiation of x-rays. Disadvantages are the claustrophobic chamber in which the patient must be placed and the excessive noise, requiring earplugs.
Functional Imaging
Positron Emission Tomography (PET) and Single Photon Emission Computed Tomography (SPECT) are similar in that they use injected radioactive material to track metabolically active areas of the brain. The radioactive material attaches to oxygen and glucose, which accumulate in areas that are metabolically active and show up as being brighter on the scan output.
in that they use injected radioactive material to track metabolically active areas of the brain. The radioactive material attaches to oxygen and glucose, which accumulate in areas that are metabolically active and show up as being brighter on the scan output.
Functional Magnetic Resonance Imaging (fMRI) combines MRI technology with the ability to see images of changing blood flow in the brain associated with neural activity. It can be used to reveal brain structures and processes associated with perception, thought and action. fMRI has largely replaced PET for the study of brain activation patterns.
Electroencephalography (EEG) measures electric fields in the brain using electrodes placed on the scalp. It does not use radioactive materials and is quieter than MRI and fMRI. A limitation is the electrical signals are distorted by surrounding tissue, particularly the skull and scalp.
Magnetoencephalography (MEG)
As mentioned above, MEG measures the minute magnetic fields that are generated by electrical activity in the brain. One great benefit of MEG is it offers real-time recording of brain activity over a period of up to 10 minutes.
It accomplishes this by means of extremely sensitive devices called superconducting quantum interface devices (SQUIDS). Because these are superconducting magnets, they require cryogenic temperatures for operation. An array of 300 SQUIDS is contained in a helmet also containing liquid helium. The patient wears the helmet in a seated position, eliminating the claustrophobic chambers of other imaging techniques.
MEG scanners are extremely expensive and there are only about 20 units in operation in the United States. They are currently used for pre-surgical brain mapping for patients undergoing surgery for brain tumor removal or epilepsy treatment.
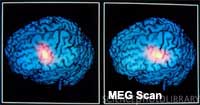
Fortunately, one MEG scanner is at the Henry Ford Health System in Michigan and Dr. Michael Seidman has conducted initial studies using MEG for tinnitus localization.1 He states, “With PET and fMRI, most of the auditory cortex of the brain lights up with activity during imaging. MEG, however, is a much more sophisticated machine and it can identify a specific tone or topic point, so only a small area in the brain lights up. It’s like having the lights on in only the city of Detroit, compared to having the lights on in the entire state of Michigan.”
For the study, Dr. Seidman and his colleagues collected MEG results from 17 patients with tinnitus and 10 patients without tinnitus. Data was collected for 10 minutes. With tinnitus patients who had ringing in one ear only (unilateral tinnitus), MEG imaging detected the greatest amount of activity in the auditory cortex on the opposite side of the brain from their perceived tinnitus. For those with ringing in the head or both ears (bilateral tinnitus), MEG imaging revealed activity in both hemispheres of the brain, with greater activity appearing in the opposite side of the brain of the strongest perception of tinnitus.
Patients without tinnitus had multiple small active areas in the brain but no particular areas were found to be highly coherent during the 10-minute MEG scan.
Dr. Seidman has used MEG scanning to find the exact location of tinnitus. He uses this information to neuronavigate to guide the insertion of electrode arrays into the brain for direct electrical stimulation of the auditory cortex. This stimulation, if placed correctly, should disrupt the tinnitus and reduce the sound levels for patients.2
In a revolutionary series of experimental surgeries, Dr. Seidman and his team have shown that an electrode array implanted directly into the auditory cortex can control tinnitus levels. It would be impossible to correctly place the array without MEG technology.
This research is very new and Dr. Seidman compares it to the development of cochlear implants for profoundly deaf people. When they were first implanted, the patient only heard a series of clicks. It took many years of biomedical engineering to provide the high quality sound perception and speech recognition that implant recipients experience today.
An article on electrical stimulation techniques for tinnitus, such as cochlear implants and cortical stimulation, can be seen here.
References
1 – http://www.diagnosticimaging.com/display/article/113619/1482978.
2 – Seidman MD, et al. Direct Electrical Stimulation of Heschl’s Gyrus for Tinnitus Treatment. Laryngoscope. 2008 Mar;118(3):491-500.
Get Free Shipping!
Order now and get free shipping on either the Tinnitus Starter Kit or Combo Pack. Try the doctor recommended products with clinically proven ingredients for tinnitus. No coupon code required.

